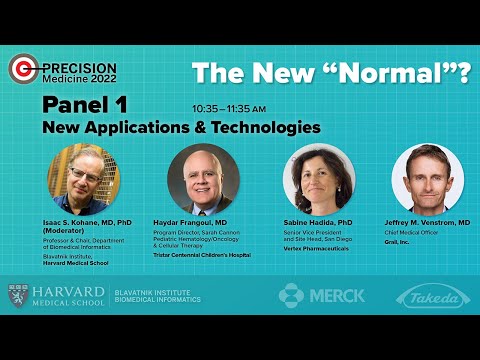
PANEL 1 — New Applications & Technologies (e.g., liquid biopsy, new diagnostic applications)
I think it's a good sign when you have to personally drag panelists from the alleyways because they're having productive conversations, but too bad. We have an agenda. And because you made me work, I'm going to make you work.
And we have a really interesting panel. But the way I'm going to make you work is going to have you introduce yourselves, right? And I think that one way to think about this panel is we just heard an amazing story just now. I think it's legitimately described as a moonshot where we worked, got the person to the moon, safely back and not only safely back, better than when they started. That's an amazing story. Are we going to be able to do this more generally? What's it going to take? Is this still going to be a moonshot like thing? I know that we've discussed already some of these questions, and I leave it to you to decide which of the questions we discussed you're going to focus on.
But each of you are going to have a, hopefully, short discussion from your perspective after you introduce yourself. So each of you introduce yourselves right before you speak. We're not going to do this in parallel. So just introduce yourself.
And then maybe I'll get a chance to ask you a question if the audience doesn't beat me to it. Please proceed. Well, thank you. The microphone works, I'm assuming. First of all, I would like to thank you for the invitation.
And I'm really honored to be here. And clearly Jimmy's story is extremely powerful. My name is Haydar Frangoul. I'm currently the director of the program at the Sarah Cannon Research Institute in Nashville. We have been involved as a team in our institution in treating patients with sickle cell disease for a really long time and as Jimmy mentioned, one of the main cures for sickle cell disease, historically, have been allogeneic bone marrow transplantation from a matched sibling.
He gave the story of the football-- of the basketball NBA player that basically did an in vitro selection finding an HLA match to his child. This is the story of every patient with sickle cell disease. Only around 15% of patients with sickle cell disease have a matched sibling that is not affected with the disease that can be used as a donor to cure the disease. So that left 85% of the patients actually not able to have any curative options or options that will alleviate their daily pain that you guys heard about. So my background goes-- I was a-- I'm a pediatrician. And you're going to say, why is a pediatrician treating a 35-year-old? It's because we are better.
No, I'm just kidding. Because-- Yes, we are. So I'm a graduate of the American University of Beirut. I went to residency at Duke University, then did a fellowship in pediatric hematology oncology and stem cell transplant at the Fred Hutchinson Seattle and the Udub and then came to Nashville and started a transplant program.
And we have been having a special interest during all this time in non-malignant diseases where sickle cell clearly is a important disease to focus on. I was really fortunate during this journey to be able to participate and open the clinical trial using CRISPR-Cas9 gene editing. And when we first met with the sponsor, and we talked about the trial, I really thought it's science fiction. It's like you are telling me you're taking the patient's stem cells out, gene editing only a single gene turning off BCL11A increasing the level of fetal hemoglobin and put it back in.
It's like, is that really going to work? And I think we participate in this trial and we were very lucky to do the first patient in the world, which is Victoria Gray which got a lot of national attention. But all the credit really goes to the patients. To Victoria, to Jimmy, to all the other patients who really participated. None of this would have been possible if Victoria did not say sign me up.
Victoria was initially referred to us for a regular good old allogeneic transplant from her half brother, and when we told her in a couple of months we were going to have a trial using your own cells, you don't have to worry about graft versus host disease, about rejection, about using somebody else's cells, but hey, look, we have not done it in a single patient. We don't know if it's going to work. We don't know it's going to help you. And we have no idea what's going to happen after we infuse the cells. And she said, sign me up. So really, I think these are the heroes that really made all of this research happen.
We are just basically facilitating it but truly the incredible courage of these patients that signed for a first in human clinical trial that proved a concept that CRISPR-Cas9 gene editing using a guide RNA can specifically target a specific gene and turn off a specific gene that will make patients make high level of gamma globin. And we were looking at her blood counts every day to see what happens after we treated her and to our surprise, she had very high levels of fetal hemoglobin. And to answer somebody's question that was asked earlier, all the patients today that we reported recently, all 31 patients, have been basically free of pain crises after this therapy. So I know it's early days. I know we need to have longer follow up but I have been extremely fortunate to work with such an amazing group of patients in my center and other centers and lead the way in a really remarkable clinical trial. And I'm hoping that-- you mean the goal is that gene editing will become available, not only for sickle cell disease and beta thalassemia, which is what we are doing now but for many, many other diseases.
I think there was a crack in the door and we opened it and hopefully many more patients with genetic disorder will be able to benefit from this therapy. Thank you very much. Can you hear me? Yeah. Just want to thank the organizers for the opportunity to be here on behalf of the Vertex Team. So my name is Sabine Hadida and I am the site head at Vertex Pharmaceuticals in San Diego. At Vertex, we focus on validated targets that address the human causal biology, and we do it in a modality agnostic way.
We use small molecules. We use nucleic acid therapies. We also use cell therapies, depending on what tool is more appropriate for the problem that we're trying to solve. I've been at Vertex for 20 years and most of my experience is in small molecule drug discovery. I've worked on two main projects. I've worked on cystic-- looking for modulators of cystic fibrosis transmembrane conductance regulator, CFTR, for the treatment of cystic fibrosis.
I've also worked on pain. And it's been an incredible honor and privilege to be part of the team that converted a science fiction idea into a therapy for the majority of the patients with cystic fibrosis. When we started our journey about 20 years ago, we focused on trying to restore the function of CFTR.
And through that effort, we discovered ivacaftor, our first medicine that targeted 5% of the patient population with the G551D mutation. Once we saw the effect of these medicine in those patients, we ask ourselves, could there be other patients that respond to this therapy? In order to answer the question, we generated some cell lines, recombinant cell lines, in the laboratory and really assess the effect of ivacaftor against these different mutations. We had the benchmark, the clinical benchmark, of ivacaftor in the clinic.
And so we tried to match that or exceed that. And with that, we were able to expand the label for ivacaftor to about 15% of the patient population. Next, we focused on the majority of patients that have two copies of the f508del. Mutation this is about 45% of the patients. And for those, we needed to add to ivacaftor another medicine that worked on improving the trafficking and maturation of CFTR to try to restore CFTR function. Through a long and winding road, we discovered lumacaftor and tezacaftor.
And the effect was really exciting for us, but we knew we could do better. And so in order to do that, we set ourselves a very, very aggressive goal to try to match or exceed the efficacy of ivacaftor in the majority of the patients with CF. And that was about in 2015. It was a pretty intense search for yet a third correcter-- a third compound that would also act as a correcter and that would improve the efficacy of our two compound combination that led to the discovery of elexacaftor. And once we discovered the compound, the sense of urgency was incredible, and it took about three years to go from first synthesis to FDA approval.
So extremely commitment from the organization and from everyone in the team to try to make it happen for the patients. Of course, if you think about discovering one drug, it's very hard. Discovering two that work together is even harder and discovering the third one was extremely hard. We had to really look for combination pharmacology.
We had to make sure the pharmacokinetics were matched, and we had to make sure there were no drug interactions to eliminate the effect of one with the other. So that's been an incredible experience and opportunity, but we are not done. We still have the remaining 10% of the population that do not have the CFTR protein, and therefore do not respond to CFTR modulators. And for those, we are targeting nucleic acid therapies. We are making great progress with our collaboration with Moderna Therapeutics, but we still have a lot of work to do and so stay tuned for more information.
Over all these years, it's been an incredible learning experience for us, and we are now trying to utilize all these learnings and to treat other diseases. And so we are working on pain, like I said earlier. We are also working on type 1 diabetes. We are working just like you heard from Jaime about our investigational therapy on sickle cell disease, and beta thalassemia apol1 mediated kidney disease, and many, many other diseases, which are at the very early stages of clinical and preclinical development.
So thank you. Thank you. Yeah, thank you. Thank you, Sabine. And I just want to also thank the organizers for inviting me to be on this panel today. I'm a medical oncologist and similar actually to Haydar, in my clinical practice, I was a stem cell transplanter.
And I actually left clinical practice as a frustrated oncologist because-- in the pre kind of CAR-T gene therapy era-- because of the lack of precision, the lack of the ability to personalize treatment decisions in the clinic and fascinated by all the ongoing research about applying both genomics and biomarker discovery and development into the clinic. And I'm currently here representing GRAIL as the chief medical officer. And a little bit about GRAIL, it was founded in 2016.
We're still a relatively new company with big ambitions to address one of the biggest challenges in global public health which is cancer, the second leading cause of death worldwide with 600,000 individuals dying from cancer in the US every year. And what we hope will be a transformative paradigm shift in cancer is a blood test that can screen for multiple cancers at once, catch cancers, both late stage and early stage and really disrupt the way we think about screening for cancers. We currently only have about five standard of care cancer screening tests out there. They're all individual tests.
They have relatively low uptake, for instance, low dose CT scan for lung cancer screening has a penetration into the population of about 10%. Partly the logistics of getting a CAT scan for screening is complicated. It only screens for one disease, whereas the technology that we've developed at GRAIL has the potential to screen for 50 plus cancers, again, with a single blood test that's based on epigenetic abnormalities or abnormal methylation patterns in your genome that's detected in the blood and is consistent with the signal for cancer. What's important for this test too, this is a screening test. It's not a diagnostic test.
It complements imaging based screening modalities, like low dose CT scan, like mammography, and we really think that it's going to be a huge paradigm shift for the way we tackle cancer. Great. Well, that was a very inspiring set of introductions.
And now as before, I invite those of you here in the audience, if you have questions, to line up. And that those of you who are online can pose your question-- post your questions, and the online team will forward your questions. So I'll ask in some ways-- well, it's an unfair question, but I'll ask it anyway. Which is the question that Jimmy gave to us, which is-- we're thankfully quite wealthy in this country, and we can afford relatively expensive therapies but there are a lot of countries which don't have our budgets. How do we imagine we are going to be able to afford the screening, the small molecules, the cellular therapies, which again, are incredibly effective, but rarely have we seen any new therapies get a lot cheaper with time in the United States.
So how are we going to address-- and I apologize because you're not-- you are people trying to do the right thing. You're a scientist at the cutting edge and you're not the marketing department. You're not the business people. But you walk around them every once in a while, and you probably have your own opinion. So I'm not asking you to represent your companies at all, but you have so much experience. By the way, I need to point out that I had a great AUB experience.
One of my mentors was Dr. Samir Najjar who was a notable doctor from AUB who trained me. All the good stuff was from him.
The bad stuff, from others. In any case, why don't we address that unfair question one at a time. So first of all, I just want to acknowledge that there is a lot that needs to be done for technologies like this to be implemented worldwide.
I think Jimmy mentioned a very important point. A small fraction of sickle cell patients are really truly in the United States. The majority do not reside in North America. So there are several challenges.
I'm not sure if you heard Jimmy but when he was born, he did not know he had sickle cell disease. So a simple test as newborn screening, which we now take for granted in the US. Every baby born in any nursery today have a newborn screening that can identify if they have sickle cell disease within two to three days after discharge from the nursery, and then interventions can be done. I was recently in a conference, a international sickle cell conference in Paris and half of the attendees were from areas where sickle cell disease is very prevalent in Africa.
And I was shocked too when they presented data that 40% to 50% in some regions in Africa of children die prior to their fifth birthday because of lack of penicillin prophylaxis, because of lack of diagnosis of sickle cell disease. So there are long ways to go. I think, yes, the therapy we are doing sounds to be very complicated it might not be applicable in areas where sickle cell disease is available. You mean, ideally what we have done is a proof of principle that gene editing can be done at least in vitro, which is we are taking the cells out, gene editing them. In an ideal world, if I have a dream, I can hopefully come to this conference 10 years from now and we can actually do this in vivo. You can basically take a drug and you can actually do the gene editing in vivo in patients, because I think if we do not-- if we are not able to move to that part where actually the drug comes in a bottle, and you just take it where the patient is and infuse it, I think it's going to be-- I agree with you.
It's going to be very difficult to make this available worldwide, especially in countries with very poor resources. And I think-- and I think what I want to say is the field has moved so far, I just want the audience here, which probably all of that CRISPR-Cas9 was first really discovered 10 years ago. And 7 years after its discovery, Victoria Gray received her first dose of a gene edited using CRISPR-Cas9. So the field is growing very quickly. And my hope is that not a very selected number of patients will be able to use this therapy, but hopefully, over time, this will be available everywhere in the world.
But it's a huge challenge, and I'm not sure I am the right person to solve it, but I can hypothesize hopefully that over time, we are able to do this in vivo. Thank you. I just want to say that the cost of health care is really a problem for the entire world, and for-- in particular, for chronic diseases. And so again, I will probably not solve the problem, but the focus of my team and my personal focus is in really trying to provide value for the patients and really trying to do better and better and simpler and simpler every time with the intent that eventually we'll have an impact in the overall cost of the medicines. Well, I think all of you are already having impact.
Yeah, Zak, I definitely share your concerns around the costs of health care by and large. And I'll say two things related to GRAIL and the Galleri test is that one, I think because it's fundamentally based on next generation sequencing that I'm optimistic that as the costs of goods, the costs of next generation sequencing continues to decrease, that ultimately our test will also ultimately-- the cost of our test will ultimately decrease. It's currently available for-- its prescription only. It's $949, which doesn't have insurance coverage currently, and we're working on that. And so we definitely take kind of the cost of health care and these diagnostic tests very seriously.
And I think the other spirit of your question really is access, right? And that's why I think, partly, I'm at GRAIL is because this is a democratized able assay or test if you can say that meaning this, because it's based on a simple blood draw, we can send remote phlebotomists which we've done actually. We can send phlebotomists to very far reaches to draw blood and to send back to the lab so that we can really democratize multi-cancer early detection for many, many patients. We actually have experience too. We just accrued 140,000 individual randomized controlled trial in the United Kingdom where we had six mobile units, buses essentially, that we would send out and we'd park in front of mosques, in front of farms out in the very rural depths of the United Kingdom to make sure that we accrued individuals to the clinical trial that were representative of the population and that weren't just easy to get to. Thank you.
So I see that we have someone in the audience. I'm going to ask all questioners to introduce themselves before they ask their question. Thanks, Zak.
My name is Aaron Abend. I run the autoimmune registry. And Dr. Hadida, your story was really interesting, because when I-- I've been following genomics for years and Vertex was really out in front with its work on CFTR and everyone was very disappointed when the first treatment was only addressing a very small percentage of the population. And that story made the news and everybody's heard that story, but nobody's really heard the story you just told which is that the follow on work, which is the hard work. Everybody wants a simple answer to these questions, but that hard work and the resulting impact that you're having, that story is not getting out there.
Again, this may be a question for the marketing department, but congratulations on your work and thank you and we need more people doing that follow on work. And the public needs to understand that medicine isn't quick fixes. Like, that's what people want, but it's all that hard work that goes into these longer term treatments. How do we get the public to understand that process better? OK.
So can I summarize? The question is, how do we get the public to understand the-- Thank you. That's a great question. It's a question that I ask myself as well when people ask me what do you do. I think the best way to do that is just to tell our story and just share that it's not a straight line from the starting point to a drug. We have a lot of ups and downs that we need to overcome, a lot of challenges. And you don't have a medicine until you have a medicine.
And so it is a long and winding road. There's a lot of investment, there's a lot of learnings and a lot of hypothesis based approaches that need to be put in place to be able to go from the beginning of an idea to an approved agent that can benefit patients. Anybody else want to take on that question? I guess I would just add what it also comes down to for me is patient safety, right? And so I think we need, as a population, to have patience for the process of drug diagnostic, screening, discovery and development because ultimately, we have to rigorously validate the clinical benefit, the clinical validation and the clinical utility of these new innovations and it's critical that we do that rigorously, methodically in a logical way. Because at the end of the day, injecting a new patient-- injecting a new drug or giving big new information like the possibility of a cancer diagnosis is risky stuff and we need to make sure we keep patient safety at the center. I-- thank you.
I see we have another question. Please identify yourself and then ask your question. Thank you.
My name is Ardita, and I'm a medical doctor from Indonesia. I wanted to ask because I've heard from Jimmy that he was initially a reserved person and then coming to your team, he even so comfortable with Dr. Frangoul and his team that he done a knee sliding on the floor. So I wanted to ask, as a researcher, clinical researcher, what is your personal approach or is there any tricks-- not tricks, probably approach to make the patients comfortable on that level? Because I believe specifically in my country, there's a lot of bias from the patients. Even they heard clinical trials, they're like, oh, I don't want that. I'm going to be for something that is going to-- a uncertain therapy.
So I would love to hear your story. Thank you. Well, thank you for the question. I think it has two components to it.
Component number one is how we make the patients comfortable. I think the main thing is believing in the patient. Communicating.
I think if you look at sickle cell disease, it has been demonized, and I think-- I know the United States has gone and continues to go through a terrible opioid crisis, correct? So I think unfortunately, the pendulum swung so hard that a patient with sickle cell disease walking into the emergency room and saying I am hurting is labeled a drug seeker. And I think his experience in our center where he was hurting, and we gave him a dose of medicine, if it is not enough we give more, I think compassion and understanding the patient journey is very important. The other thing I think which is very important that Jimmy has mentioned is how can we make this story-- other patients, kind of, pursue this? I can tell you that neither a presentation at the American Society of Hematology nor a New England Journal paper brought us patients.
Actually what brought us patients is Jimmy going on the BBC and doing an interview and Victoria Gray going on NPR and telling her story. People want to look at patients looking like them, experiencing the same thing they do, telling their story and telling that this is a therapy that potentially can help them. I think it goes a long ways to bringing patients to more clinical trial. You mean, I can come in to this meeting and talk, I can go to national meeting, we publish papers and none of that made my phone ring off the hook.
Jimmy going on the radio and Victoria going on the radio station, going to advocacy groups and telling their stories is what really is bringing patients to these trials. I think that's incredibly important, and those of you in the audience who are science writers in the popular press, I concur in our work in the undiagnosed disease network. I can tell you, the patients are far more powerful voice than doctors or scientists. I see we have another question from the audience. Please identify yourself before your question. Hi.
I'm Hannah. I'm part of the biomedical informatics master's program here at Harvard and previously, I worked at a company called Owkin which was looking at AI driven diagnostics for oncology. So my question is mainly towards Jeffrey. So you mentioned like the number 50 plus cancers as part of the cancers that you're targeting. I was just interested to know how you've gone about prioritizing which cancers are part of your test. Whether it's entirely feasibility driven, or whether there are other considerations you've made there.
Great. Yeah. Thanks for the question, and really, we let the biology and the science drive the decision making for what product ultimately we took to market. So some of the history a little bit in the test development. We took more of an agnostic approach with the hypothesis that maybe mutations or SNVs, maybe chromosomal abnormalities, maybe methylation changes would be the best way to screen to detect particularly early stage cancers. And we did a head to head study and we published this in peer reviewed papers to demonstrate that it's actually the epigenetics.
Somewhat surprisingly, at least to me, there's relatively newer area of cancer biology. We've been able to just define and determine a key hallmark of cancer. One of probably the newer hallmarks of cancer that is shared across all cancers.
This abnormal methylation pattern that we've developed and then put into this Galleri test product. And that's really how we made the decision. And so it's not specifically choosing one cancer or another. It doesn't have to be because there is.
It's the next generation sequencing platform that captures the methylation changes and then on top of that, it's artificial intelligence and machine learning that actually determines that this pattern of methylation is abnormal and consistent with cancer and that pattern of abnormal methylation is actually shared by multiple different cancers. There are other components which again, I think this is fascinating technology. This is why I'm here at this company because there are other components of the methylome of the epigenetic modifications to the DNA that we capture that can also give us insights into the signal of origin.
So whether or not that is a cancer. It's a common cancer signal, yes or no. We get that information. And then we can say actually is it more likely to be a cancer of the lung? Is it more likely to be a cancer of the colon? And give additional information on our simple test report that we give back to providers about whether the diagnostic workup should probably be directed in this specific way. So it's really all about the methylome, the epigenetic alterations, and that was discovered through a rigorous kind of head to head comparison of other genomic capabilities for screening cancer.
Thank you. I see we have another question from the audience. Please identify yourself and then your question. Hi I'm Carlos Bustamante from Galatea Bio in Stanford.
So I'm an unabashed GRAIL fanboy and a happy customer, right? Best $900 I ever spent. Lucky negative last time I took it, and I'm going to take it every year. And to your point about faster, better, cheaper or maybe my interpretation of faster, better, cheaper, I think the only way to get this broadly available is to make it a consumer product that you can order directly up. So if you're the Apple, right? Let's imagine you guys are kind of right now the high end of the market, do you see a kind of Google version and Android version that puts it out there, number one? Is the data available that would kind of make it broadly available so that hopefully you could have some good knockoffs. And then second, could there be liquid biopsy for everything else aside from cancer? Could you do long haul COVID? Could you do these other areas, and what are your thinkings? You don't have to speak on behalf of the company, just in general about lateral directions that you could go.
But in general, thank you for the product. I think it's an awesome product, and I think you're doing God's work. So thank you.
Yes, please share your business plan with us, the secret plots. And the R&D. And R&D. I'd like it. Absolutely. And your answer. Yeah, no.
It's a great question. I appreciate the complement too. So first, we take-- again, getting back to my point about patient safety. This is serious stuff, right? When you're trying to give a new diagnosis of cancer to an individual who maybe has no prior history of cancer. The clinical trial that we just read out called The Pathfinder study had 6,600 individuals that were asymptomatic and had no prior history of cancer and by and large and we were able to detect cancer in them.
And so currently, we've made the decision to require a prescription, to require that conversation with your primary care doctor because-- for multiple reasons. Again, because of the potential risk that we could get a false positive. False positives happen with every type of screening study. And having that conversation too in the context of what are my risks for cancer? Am I still smoking? What about my weight? And having that conversation with your provider when you're ordering a cancer screening test that's new, I think is really important. And the other reason why it's currently by prescription only too is that follow on.
Is it requires-- it's just a screening test. It's not a diagnostic test, meaning additional perhaps endoscopies are required to confirm the presence or absence of cancer. And so it needs that careful rigorous follow up.
Not only that conversation around what are your risks for cancer and what is the likelihood that this will be valuable for you shared decision making but also that follow up of the diagnostic odyssey and journey. So currently, it's by prescription only. It could change in the future. There's nothing on our specific business plan or roadmap that I'm aware of. But because of patient safety, and because of the reasons that I just described, we currently anchor to a prescription only. That said, to your point again, I also share that urgency.
This is a disruptive technology that really, again, we hope will also democratize the way cancer is screened across the world. And as we've seen with restrictions that have lightened in terms of telemedicine and being able to have a license-- a medical license that crosses multiple states, we do have a telemedicine portal, and so I think that's also another way, again, where you're connected with a provider there and then actually after your test, if the test comes back positive, you can connect with some world experts at academic medical centers to help you understand what that test result means, how they can potentially get that next phase of the workup, which would potentially be imaging, CT scan, MRI or endoscopy. So that's one step that we're taking closer to, I think, your sense of urgency as well, which I share of trying to get this even more broadly out there. So thank you for the answer. And unfortunately, you just touched one of my hot buttons. Briefly during the COVID, we actually, as a society, removed the barriers to practicing medicine across state lines for telemedicine.
Now for all the bad usual reasons, those limitations are coming in back, and you have to be licensed in the state that the patient is in. So that's very unfortunate. I see someone from our audience has a question.
As per usual, please introduce yourself first before you ask your question. Hi, there. My name is Ralph [INAUDIBLE]. I'm a I'm a medical student here, and I'm helping with the conference. So we've got a few questions from the online attendees. Oh, thank you.
Yes, yes, yes, yes. So they're not my questions, but yeah. So I guess we'll start with this one. How do you convince patients that the way is long and winded and face-- considering the recent developments with the COVID vaccine? And my interpretation is that the COVID vaccine didn't like-- people removed a lot of barriers to get it to work so quickly, and yeah, so how do you-- So I'm going to ask Dr. Hadida to first answer that question. So how do you talk to patients about the fact that there's a long and winding road given this apparent like overnight win with Moderna's and others vaccine? And could you add to that, perhaps, the interaction of the patients in your particular long and winding road? Yes.
Thank you for the question. This is actually a question that is very close to my heart because we've-- and I'm going to come back to our experience in the cystic fibrosis world. We have worked with patients all along. Patients have helped us understand the problem. They have-- I'm going to give you a couple of examples. Initially, when you think about CF, is the lung that comes to mind.
And so you would think of an inhaled therapy. The first-- the reason why we went with an oral agent is because we talked to the patients, and they told us we take so many inhalers, we don't want to take another inhaler. If you can give us a pill, that would be much easier for us.
And through that interaction, we were able to provide a product that not only addresses the challenge of the malfunction of CFDR, the level of the lung, but also in a systemic manner. So I think the patients play a really big role. Another example I can give you is-- and this happened to me in my-- I think it was 2003, so quite some time ago.
We've-- for all these years, we've had families come and visit us in the lab. So at the time, I was the chemistry lead for the cystic fibrosis project, and I had this family with a little girl. She was probably four years old so I had set up-- I had organized a whole thing for her. We had all the automation working. I was trying to explain to her what we were doing in the lab to try to find a medicine for her.
After I finished with all my show, she looked at me and she said this is all great, but where is my medicine? And so I think this is what the patients do to you. They really give you the focus. They give you the drive, the sense of urgency, and they also-- it also allows to have a face to the problem. When you face a roadblock, I always remember this little girl looking at me and asking me for the medicine. I think the sense of urgency is one that we, with our busy lives, tend to forget.
So I think that's absolutely crucial. Anybody else want to comment on this? Yeah, I mean, just really quickly. I guess I agree.
I mean, I think I was so inspired by the speed of rollout for COVID vaccinations, and I was also asking myself too. And I've read there's quite a few books out there about the reasons why or some of the underpinnings of that and to me, it comes down to three things. One is collaboration. I think even on the manufacturing side for some of these vaccine, we saw companies that normally compete actually collaborate to get these vaccines out. So collaboration to me is fundamental and doing it quickly in an agile way with huge public support. The second thing is regulatory too.
So we actually have, for our test, FDA breakthrough designation which gives us access to have multiple conversations with the FDA as we're developing our clinical validation, as we're designing our specific studies for clinical utility. And so I think the regulators are also appreciating this sense of urgency and understanding that this is really important to get to accelerate that pace of innovation. I think that's, to me, fundamentally, the source of the question. And then the third pillar I would say here is patient advocacy.
Absolutely. I couldn't agree with you more. And I wanted to make that comment to one of the earlier questions too just the importance of patient advocates.
I mean, it really heralds back probably before, but what I remember to like the HIV days and the crisis and how patient advocates during that crisis was really able to help expedite and focus research dollars and focus development efforts. Thank you very much. So if you want, we can ask-- we can answer a question first and then I can-- Go ahead.
Oh, OK. Hello. My name is Harriet. I'm currently a research technician working in Dana-Farber in the oncology department. So today, my question would be toward Jeffrey.
You mentioned you did this transition from the clinics-- very frustrating-- to industry. So I assume you have some experience in both sides. So my question would be on your insights on oncology research to drug discovery, to the clinical trial, to the eventual listing of the drugs on the market. This procedure usually takes a really long time before the drug actually going on-- going to be listed on the market and eventually being applied to the patient. Do you have any opinion on speeding up this procedure? So a couple of things I think there.
One, I think was a question just around my journey too and I'm just a super curious person too, and what I experience in academic medical-- in my academic medical career is the focus on, essentially, grants and publications at least from the science side. And really what I was most passionate about is trying to understand and figure out how to move a concept to a product that you can prescribe in the clinic, and I was exposed, again, I was actually on faculty at the University of California, San Francisco and Silicon Valley. It's pretty easy to get access to biotech or friends that are in the industry trying to do their thing. And I got very curious about the regulatory process. Like how does-- what does it take to actually get either a diagnostic or a drug approved? And so that was a major, kind of, decision point also in addition to my frustration and the opportunities for developing biomarkers, discovering biomarkers and personalizing therapies that I saw was happening a lot in industry. So that was really, kind of, the origin for my transition from academics to industry.
And then your second question I think relates to what I had mentioned earlier to the online question is around collaboration. I think your question relates to speed collaboration. What we've done for this Galleri test is collaborated with dozens of academic medical centers and partners, including Sarah Cannon for really getting this test validated and actually getting access to patient samples and being able to really think carefully and clearly about the design of our studies. Again, working closely with regulators, working closely with patient advocates too and trying to really understand and design studies and tests or design trials that are relevant for patients, relevant for the regulators. And so really putting all that together as your clinical development plan, I guess, for a specific product in a very kind of collaborative but also expeditious way is how we've approached the speed question.
Oh, that's very informative. Thank you. By the way, in a creepy and impressive demonstration of machine learning, looking at my Twitter stream, global Blood Therapeutics Incorporated just injected an ad into my Twitter stream informing us, did this-- that it's sickle cell Awareness Month. It is.
And that-- There we go. All right. Wonderful wonderful. Thank you. So our next question from the online world is directed towards Doctor Venstrom. How are we going to change the paradigm as you are hoping to do in the question askers field, breast cancer? The field is monetized and monopolized by radiologists.
And there's a follow up comment. Any new innovation in breast cancer screening is another imaging test that may add a small improvement in accuracy, while being much more expensive. So let me try to broaden the question so that every one of our speakers can answer. There is a detection part of each of these stories, and who is the right holder of that detection function? Is it, as you suggested, perhaps public health with neonatal screening? Where is the right locus? Who should be responsible for that detection function? Well, I can start by saying that it depends on the disorder, correct? When you look at disorders that-- as a pediatrician I deal with where early detection means early intervention, great examples are sickle cell disease, immune deficiency where we are now doing newborn screening for immune deficiencies. I think some of those screenings need to be done in a massive amount and you have to do them at the public health level as compared to what Jeffrey's stuff is going on to detect cancers later on in life.
The other thing which-- I know I'm not supposed to ask questions, I'm supposed to answer them-- No, go for it. But my question about screening for some disorders is the impact on the patient and their ability to get insurance, their ability to afford health care, how is that going to impact when we do screening, yet it's great, correct? You can screen. But what's your plan what to do with that screening and how it will impact the patient? And I think these are all interesting questions we all need to ask whenever we develop a screening test. Might that be a newborn screening for sickle cell disease or a screening for breast cancer or colon cancer, correct? So I think it has more implications and I think all of us need to think about how to make it better for patients and protect them from things that some of the screening tests will make it more difficult in their life.
So because-- I have to admit, I guess I just have a nasty streak in me. I'm going to ask Jeff to both answer that question, but answer that question, which is-- God forbid someone they are at high risk for cancer, they don't have a whole lot of insurance and they're in these surprise insurance clinics that are all over our country. What kind of service are you actually performing? So yeah, I guess I'll take both questions.
One, I think for the online question, it sounds like it's really anchored, to me, to an opportunity for education too, right? Like the question, I think, originated in the standard of care for breast cancer screening, which is mammography which is run by a radiologist. It's a very different modality and very complementary modality to what we're trying to do, which is a blood test for breast cancer and other cancer treatments or diagnoses. And so one again, I think we're completely complementary with the imaging technology. So we're not trying to replace radiologists or fight with radiologists. We're really trying to-- Why not? Sorry. [LAUGHTER] And the second piece is we never know what cancer we're going to develop.
Again, one in two or one in three of us will be affected by cancer, and many of us have been affected by cancer in our family members. And so you can't predict whether or not you're going to get breast cancer, prostate cancer or colon cancer. And so again, that's where the potential differentiation or new opportunity that this test really provides is using a simple blood test, being a little bit agnostic to your specific risk factors, whether or not it's for one cancer versus the other. So again, this is a completely different way of thinking about individual cancer screening versus multi cancer screening.
And that's fundamentally based on the fact that we don't know what individual-- I mean, for some, of course, we do but oftentimes even those genetic alterations, you're susceptible to multiple different types of cancers. And so that's why we think this new test has great potential and power. Absolutely.
And we monitor this very closely. So again, it's a prescription only test. We've now rolled this out to around 40,000 individuals or patients that have ordered our test and we're constantly monitoring and asking that question. We provide resources to help both the provider and the patient understand insurance coverage and next steps for that diagnostic piece. It's useless, right? This test is useless if you don't have that follow on imaging. And we actually-- we haven't found any challenges with actually getting that positive test for the 1.4%
of the tested population that becomes positive or that is detected positive and getting those follow on diagnostic tests. We're also, again, a new fast company that's trying to move quickly. Only founded in 2016.
And so we're now establishing our financial assistance program too for those that also-- again, anticipating that gap that we currently haven't faced with the current rollout of our test. Thank you. Things are piling up so we're going to increasing the pace. So please introduce yourself and question. Hi.
Stanley Shaw. Harvard Medical School and Brigham and Women's. Can I ask about if we need to do, as a community, better to make the value appearance of the innovations that you all represent, right? So we have two therapies that arguably don't even need much of a sales force. The value to patients and families is so strong but they're expensive, and I know you've-- Vertex has fought some battles with nice and things like that. On the other hand, at GRAIL, you potentially may have to run a gauntlet of not just the accuracy of the test but how it contributes to screening.
And you obviously don't want to end up like PSA or we don't want to have an elegant PSA analogy 10 years hence. And so how should we be marshaling evidence to make the argument to health technology assessors so that these can be paid for and folded in? And I think if there's less uncertainty about payment then doctors are probably more likely to do the screening tests and to go looking and to treat. So let me ask Dr-- let me ask Dr. Hadida to first answer that question because Dr. Shaw is absolutely right.
Incontrovertible value to patients. But if I'm public health, I can say with the cost of a CF treatment, how many babies could I screen for this disease? Could I treat with asthma, and so on. So let's try to make concrete, how do you make that value proposition public? What kind of evidence do you use? Thank you. Yeah. So in the case-- and I'm going to bring it back to the case of the cystic fibrosis case where the CF is part of the neonate gene screening.
And so before birth or at birth, parents know that their child has CF. And I would say that the Cystic Fibrosis Foundation has done a really good job really building in a registry of patients and building in some centers to try to treat patients as early as possible. So there's a whole network that is in place to be able to address the disease. And sounds like doubling down on the role that patient advocates have for making that value proposition. Anybody else want to make a comment? The health economics of some of those treatments, although we are talking about them, we don't, again, we don't set the cost.
But think about more than $1 billion spend a year on caring for patients with sickle cell disease in the United States, correct? This is the-- the economic impact is very high, and that does not account for lost wages, for missing work, for missing school. So I think all of these therapies, you can make a very easy economic decision that the therapies cost really is a fraction of what's going to take to care for these patients long-term. I agree. And I think that we saw how much we were willing to spend as a society in COVID and very fast in large amounts. Imagine what we-- would have been ready to spend if we would have had the time to a vaccine. So I agree.
Go ahead. My name is Caroline Dennis and I'm an entrepreneur. And I am also working at the intersection of blockchain and health care and AR and VR. My question is really focused around a lot of comments about democratizing collaboration. And I spent yesterday at an organization that has created an open source tool for looking at data and AI. I guess my question is more philosophical than anything else, but do you see a time where our centric focus on keeping data lakes and data fiefdoms is going to change into a place where we can actually really share data freely? Because I think we are still at a place where people develop data and they are still not necessarily sharing that data.
So if we are going to push ourselves to that place where we can have a world where things are more affordable, do you see that happening and if you do, do you see any possibility of that happening anytime soon? Maybe my attention wavered. Was the focus on the data sharing part of it? Yeah. I think that there's a lot of data that moves around. Data gets shifted, copied, pasted, and we now have technologies in the blockchain space. We're seeing it happen all over the place. But I think there's still this idea of people coveting their data.
Haydar, in your trial, what do I need to do to find the data on your patients? Well, we are very transparent in our data when it becomes available. We present it at the earliest available opportunity. And we are hoping as we accumulate more data-- and I think I agree with you. I think some of these studies, even our study that we are doing, is accumulating data that is not part of the end point of the clinical trial. And in fact, it's very timely because I had a meeting yesterday with Vertex who is the sponsor for our trial, and we talked specifically this, at how important it is to share of this data that we are collecting massive amount of data that is not part of our end point to make it more available to the community and what is happening to the patient.
I'm in total agreement with you that the more transparency and data sharing, the better all of us. Because I'm cognizant of the fact that we're down to the last minute, I'm going to ask the person behind our student, you, to identify yourself and ask a question, and it will be the last question. My name is Carly Smith. I'm a graduate student from MIT in the department of mechanical engineering. And I had kind of a two part question.
At what point are the operational challenges of implementing these new technologies into clinical practice considered? And then the second part of that is who becomes responsible to identify and then integrate the technology safely and accurately? I think those are pretty good questions, and I'm actually thrilled that we have mechanical engineering students at this conference. That's a very good sign for a variety of reasons. I'd like all of you to take a whack at that question.
Haydar, want to give it a shot? My first attempt is I think there is a learning curve to all these clinical trials. What Jimmy mentioned about his experience with collecting peripheral blood stem cells from a patient with sickle cell disease is challenging. But I think as all of us become more experienced with this and we work out the kinks in all of these issues to make it easier, I think we can disseminate that information to everybody doing clinical trials for sickle cell disease patients to make what Jimmy talked about how challenging it is to collect these stem cells, for example, to be much easier in the second generation trials, or even when this becomes commercially available. So I agree with you. I think it is very important for all of us in all the fields we are in to learn as we go.
Not only learn but also disseminate that knowledge to other places to make things much easier and much more streamlined. I hope that answers it. Dr. Sabine, you mentioned the pill and what did it take? How did you think of operationalizing that? Oh. It took an army. It was a significant cross-functional effort to be able to get from the idea to that pill.
Actually I just wanted to bring up that we actually at our site, we work with a group of engineers that help us really build specific types of equipment to be able to generate the type of data that we need to be able to deliver those pills. So it has been an incredible effort from even getting the tissues, culturing the cells to be able to measure the activity of our compounds all the way to being able to co formulate three compounds into a single pill. Great.
And Jeff, there's-- especially for not purely genomic technologies for something like methylation, there's a lot of handling stuff. How did you consumer safe your technology? How do you think about it? I love that question and absolutely-- I mean, operational complexity is front and center when you're developing a test particularly as it relates to cancer or the possibility of cancer when patients are waiting, you have your blood drawn and that turnaround time is one kind of component of the operational complexity that we really look at very closely. And we always have an annual goal of trying to decrease the turnaround time, trying to understand and look at every component of the process that's required from blood draw to result reporting and what our areas and opportunities where we can shrink that-- where we can decrease the complexity of the operational workflow and shrink the time that it takes to actually run this test. So operational complexity is something front and center. And another good example is, as we think about how best to improve our test, there's a hypothesis that adding urine, for instance, in addition to blood or adding proteins in addition to methylation could improve the test and we're very cautious, before we ultimately make a decision to change our product, that we consider the operational complexities of adding another analyte like urine or adding another component of a test.
We think that currently the way the test is running is a simple methylation assay that requires complex computational biology, but focusing on that, that one key hallmark of cancer is the best way to decrease that operational complexity, get the result back to your patient fast and be a world class product. Great. I apologize.
I know there's many more questions. Thank you for that question. Thank you to our panel.
That was a really wonderful discussion. [APPLAUSE]
2023-08-31 04:13

