Mapping the Path to Relief: Improving Pain and Opioid Use Disorder Through Neuromodulation
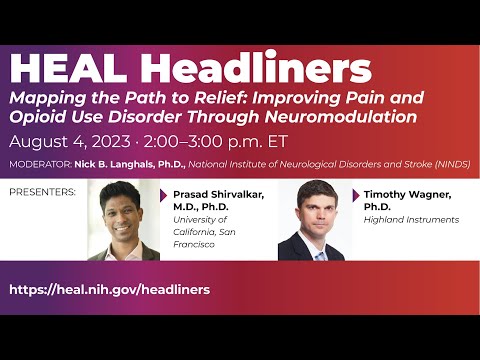
NICK LANGHALS: Welcome everyone. Good afternoon and thank you for joining us today for the HEAL Headliners webinar. As mentioned, I'm Nick Langhals from NINDS, and I have the responsibility and the privilege of helping to moderate this session today. We're all aware that new safe and effective treatments are needed for people living with chronic pain and or opioid use disorder. Today's webinar will highlight the work of two heel funded researchers who are
making strides toward achieving this goal. By using neuromodulation as a novel treatment approach for chronic pain and opioid use disorder. Although our two presenters are using very different technologies, they both seek to treat chronic pain and opioid use disorder by targeting and resetting the neuronal circuits altered by the two conditions. Our first speaker today is Dr. Timothy Wagner. Dr. Wagner is the Chief Science officer of Highland Instruments and a lecturer at the Harvard Medical School and Massachusetts Institute of Technologies, Health Sciences and Technology Program. At Highland Instruments, he leads the team in the development of Electrosonics stimulation or ESTIM technology, which is a non-invasive technique that is being tested to treat chronic pain, opioid use disorder, and Parkinson's disease. At this point, I will turn it over to Dr. Wagner for his presentation.
TIMOTHY WAGNER: Hello. Let me get the screen up and everyone in. Hello. So can everyone see the screen? LANGHALS: Yep, looks good. WAGNER: OK, great. So let me just start by thanking everyone for listening today and the NIH for championing the HEAL Initiative. Over the next 15 minutes, I'll give a brief
overview of the field of neuromodulation focused on non-invasive approaches and applications to pain and substance abuse. And then I'll describe a new form of non-invasive brain stimulation that we are developing called ultrasonic stimulation or ESTIM for short. And finally, we'll briefly review two heel studies that we have underway for chronic pain. Now, coming from an engineering and physics background, I like to think of brain stimulation as the application of energy to the nervous system to modulate function. This
can classically be exemplified through an invasive electrical energy example where an electrode is surgically implanted in the brain. It is connected to a power source and it injects currents into the neuro tissue to activate voltage gated ion channels in the targeted cells to stimulate them and ultimately modulate neuro function and the neuro network activity. So while the intricacies of stimulation can be quite complex, there are a few key points that should be highlighted. Dependent upon the applied energy's intensity, spectral pattern, location, and temporal characteristics, energy can impact cells and networks in numerous ways. Stimulation can make a neuron actively fire. It can alter the excitability of a cell,
inhibiting or facilitating the likelihood the cell will. Fire stimulation can be used as a source of noise to disrupt normal or abnormal function. It could be used to alter brain oscillation. It can be provided over different time courses. It could be provided continuously or intermittently with repeated sessions with gaps between sessions that can last from weeks to months, an induction in maintenance phases. Now, stimulation can be
provided in a way where the modulatory effects are seen during stimulation. This is called online effects. It can also be provided in a way where stimulation lasts past the duration of stimulation, which is referred to as offline effects. Now, when these characteristics are appropriately leveraged, neuromodulation can be used in a therapeutic manner whereby stimulation can be used to treat neuro pathologies marked by a network imbalances in targeted brain centers. Today, brain stimulation techniques such as invasive techniques like deep brain
stimulation and non-invasive techniques such as transcranial magnetic stimulation, transcranial electrical stimulation, and transcranial ultrasound are becoming more common. The developmental trajectories of brain stimulation in the pain in addiction spaces have both advanced from animal to human use and included both invasive and non-invasive approaches. Today, there have been over 100 human trials exploring non-invasive brain stimulation in chronic pain, and non-invasive applications in addiction are rapidly evolving. While both trajectories are fascinating, and we could spend the day talking about them, I just want to focus on one of the common themes across both trajectories, and that's the general result that invasive approaches are usually more efficacious, but at the price of invasiveness. So generally, invasive methods have superior pocality, targeting control penetration dosage control, which translates usually into a larger or a greater neuromodulatory effect or longer neurologist effect at the expense of invasiveness. And this is really been our motivation, and we've
been exploring methods to develop improved non-invasive technologies. We're exploring methods to couple technologies together. For example, ultrasound has superior focality penetration and targeting control compared to electrical methods, but is not shown the same neuromodulatory effect as electrical methods. So we asked the question, can we couple them together for an advantage? Can we use the techniques together and use the advantages of each? So continuum electromechanics provided us a clue on how one might combine the energy as can be demonstrated from a simple circuit example. Now, I apologize for those
not familiar with circuit theory, so please don't tune out as I'll only spend about 10 seconds on this. But I think this is key to some of our early thoughts on how these technologies could be combined. If you look on the left side, you'll see that the circuit, when a capacitor is exposed to a DC voltage, the current across it is zero. However, if one imparts of force on the capacitor and modulates the dielectric, one can see an impact and generation of a current, proportional to that change in capacitance. So that's the idea
behind electrotonic stimulation. That one can combine electrical and ultrasonic energy together to generate or alter the stimulatory currents. It so happens that brain capacitance, you can modulate it or modulate it relative to the electric field and alter the stimulatory currents or alter the effects. So that was our hypothesis. So fundamental physics supported our hypothesis that electro mechanically coupled energies could be used to focus, amplify, and direct the stimulation currents. But really beyond the one second, I am having a bit of
an issue. OK, so you should see this combined energy slide at the moment. So, you know we started with, you know, the fundamental theory supporting the concept, and we began by conducting a number of preclinical experiments, including histology, electrophysiology, behavioral and imaging studies. But one simple experiment, really and this is the experiment that I'm going to review rather quickly, demonstrates the difference in our technique and others and the impact it can have on neuro cells. So what I'm showing here is the results of a study we conducted, a preclinical animal study where we implanted electrodes within the visual cortex of animals, and were assessing the impact of stimulation on a visual evoked potential in the animals. We looked at sham stimulation, transcranial ultrasound stimulation, transcranial direct current stimulation, and SSTIM or ultrasonic stimulation, which combined the two energies in a dose equivalent manner. And what we saw was quite fascinating. We
provided transcranial ultrasound in a way that suppressed activity. We provided the electrical stimulation in a way that could enhance activity. But when we coupled the two together, we saw this amplification of effect and in the direction of the electrical stimulation source. Now, we also saw significantly greater effects compared to electrical and
ultrasonic stimulation in depth and on the duration of effect. So you know, this was actually years ago, years ago when we did this, but we knew we had something. And fast forward to today, after years of further preclinical testing, we now have a number of clinical trials that have been completed or underway, some in chronic pain indications like diabetic neuropathic pain, but also including indications unrelated to pain or substance abuse like Parkinson's disease. And here I'm showing you a rendering of one of the systems we are developing, a simple patient worn system that allows the application of electronic stimulation. But now I want to spend a few minutes reviewing two clinical trials, we have underway supported by HEAL. They're going into the phase two portion, but I want to review the feasibility components of the trials that were just recently completed. And I'm going to highlight aspects
of the phase two trials. So the first trial that I want to talk about is our carpal tunnel syndrome study, but let me speak overall about both the design of both studies. So they were both conducted in two separate phases, essentially with the first trial to assess the feasibility of SSTIM in the indication and the second phases are ongoing right now of the trials with larger patient cohorts, increased stimulation visits, extended testing and follow up. So they're following a paradigm of phase one, assessing feasibility and phase two in a much larger trial. So the first trial, we were assessing the impact of SSTIM on chronic pain and carpal tunnel syndrome. So carpal tunnel syndrome is a significant impact on the country.
It affects some 4% of the population. Neuropathic pain is one of the most common and difficult to treat complications of carpal tunnel syndrome or CTS as I refer to it. Given that most conventional treatments at the neuropathy site. Although CTS has a central pain component due to the injury, we hypothesize that SSTIM directed at central pain centers could be effective as a non-pharmaceutical adjunct therapy in these patients. Furthermore, we're coupling this SDM treatment with physical therapy. While physical therapy can be effective in these patients, pain can limit patients' compliance with protocols. And there's also a desire
to develop more effective PD regimens and protocols. So we've hypothesized that appropriately applied SSTIM PD could work together synergistically. So in the feasibility phase of the study, we recruited 20 patients with chronic CTS pain involving at least one wrist. They had chronic pain as defined by the International Association for the Study of Pain. The average baseline pain on a vast score was a 5.5, and patients were not responsive to first-line
therapy. Patients were randomized between the active and sham groups and 10 per group. So we implemented a simple protocol on these patients where patients just underwent five days of stimulation, 20 minutes per day, and completed follow ups up to six weeks post stimulation. We assessed a battery of safety, pain, quality of life, quantitative sensory testing, and biomechanics based testing. So the study, it was, you know, focused on feasibility, but we tried to be comprehensive in our assessments. The one thing I want to note before I talk
about when we're moving to phase two is in phase one, we did not couple physical therapy and that we are doing that now, so we will not speak about PT and phase one. Now, this trial, first of all, was safely conducted. It had a similar safety profile. It's transcranial direct current stimulation. We demonstrated an impact on the quantitative sensory testing measures, which were indicative of a change in the diffuse noxious inhibitory control through a CPM measure. We demonstrated approximately 25% reduction in pain average in the period following the last stimulation through the last follow-up. The figure on the right corner, those are improved vast pain scores from baseline in the period from the last stimulation average due the last follow-up. We also demonstrated significant effects in the neuropathic pain
symptom inventory, and the Boston Carpal Tunnel questionnaire, and supporting the hypothesis that PT and ESStim can be coupled together, we demonstrated improvements in biomechanics. Here I'm just showing an improvement in reach-to-pinch mean speed from baseline in these patients. So ultimately be concluded that the concept of coupling ESStim with PT in carpal tunnel syndrome is feasible. So we currently have a phase two trial ongoing, looking at 60 physicians now providing ESStim in conjunction with physical therapy, over 10 stimulation sessions with 10 PT sessions over three week period and follow-ups up to eight weeks post-therapy. Now on top of conducting the trial, our goal is not only to validate the technique, but we're also developing models of the stimulation effect to optimize therapy. Our goal at Highland Instruments and the goal of the team that I work with is to optimize the therapy for the patients and with a long-term goal of individualizing therapy for the patients based on patient's baseline, parameters, and elements of the stimulation that we are giving. So
with that said, we have a phase two trial ongoing. Now I know my time is almost up, so I will go rather quickly, but I want to talk about a second trial that I'm very excited about and it follows the same paradigm earlier where we're using a phase one and phase two, and phase one was focused on feasibility. And I will just shortly say as you know, there's been a history of NIPS devices for treating substance abuse disorder, and in this light, we are conducting a trial to assess the impact of ESStim on opioid use disorder or OUD. And I should mention, and I should have mentioned it earlier, that we- So we're conducting this study in conjunction with the University of Illinois, Chicago, Case Western Reserve University, and we're about to add one of our sites at Harvard Medical School as a third site. And
we've had a tremendous amount of help from the local methadone clinics who've helped with this study and they've significantly helped us and contributed, and I really feel honored to be part of their community. Now, like the above program, we we're conducting this in two phase. The first trial, which is completed, focused on feasibility, and the second trial has expanded accordingly. As previous, I'm focusing on the feasibility study. So we assessed patients with a diagnosis of OUD who still feel craving, 95% of which came from the methadone clinics, and that I said were instrumental to the trial. So we provided patients five days of stimulation, 20 minutes a day, and conducted two follow-ups at one-week post-stimulation and one-month post-stimulation. As above, the trial was
safely conducted and we had a similar safety profile to TCS. The primary endpoint in this study focused on patient craving, which demonstrated a large, significant effect. Here I show again the average change in craving from baseline from the last visit through the last follow-up. We demonstrated effects on secondary end points as well, including a measure of impulsivity, patient drug use if that's the day we were in toxicology, and we ultimately concluded that the concept of using ESStim and OUD is feasible, and we have a larger phase two trial underway. So in the largest phase two trial, we're feeding for up to a hundred patients, we're filing patients for up to six months. Our goal is, again, not to only validate it, but to understand the technology and to ultimately be able to optimize our treatments for these patients. So in conclusion, we've gone over brain stimulation just globally as an application
of energy to modulate network function. We reviewed that there's both invasive and non-invasive approaches that have been used in the pain and addiction fields. We've reviewed Highland instruments, electrosonic stimulation or ESStim technique, and a number of the trials that we have ongoing in the chronic pain in opioid use disorder space. And most importantly, I just want to thank the NIH, the Heal Initiative, the Highland team, my team is great. My co-PI
Laura de Pietro has helped considerably, and the other team and collaborators from Harvard Medical School to Case Western Reserve to the University of Illinois, Chicago, across all the institutes have all just been exceptional and we've enjoyed very much working with the NIH. And I'd just like to thank everyone for listening today. LANGHALS: Thanks, Dr. Wagner. So as a reminder for those that missed the introduction, I will hold the questions after the second presentation. If you have the questions that you've come
up with along the way, feel free to put them in the Q and A section at the button at the bottom of your screen. So our second speaker today is Dr. Prasad Shirvalkar. He is an associate professor in the Department's Anesthesiology and neurological surgery at the University of California San Francisco. He is a neurologist and interventional pain medicine specialist. His research aims to apply technology-based therapies for hard-to-treat pain disorders such as post-stroke pain and phantom limb pain. Prasad take it away. PRASAD SHIRVALKAR: Thanks so much, Nick, and again, it's an honor to be here. Hello, everyone, thanks so much for tuning in. And in the next 15 minutes, I'm going to talk about our HEAL initiative-funded project that really aims to develop adaptive or personalized brain stimulation therapy to treat refractory chronic pain. As a brief introduction, we started
this off with a brain initiative project, which morphed into a HEAL initiative project. So it's actually, there's two clinical trials that are ongoing. These are my disclosures. Everything I'm talking about is off-label funding from the NIH HEAL Initiative, Brain Initiative, and some private sources. So first, I'll talk about why chronic pain and why brain stimulation may be a promising avenue or a promising approach to actually treat and change the course of chronic pain perception in individuals. I'll talk about a recent study that we published that shows for the first time that we can actually detect and track real-world chronic pain signals. And then I'll talk about our ongoing clinical trials that aim to use these signals to actually feedback and control brain stimulation. So you all are very familiar
with the urgency and the importance of treating chronic pain so I won't belabor to the point. I think it's notable and for me, frankly surprising that actually- The first study actually that rigorously evaluated I think in a large population, the incidents and persistence of chronic pain was recently published in May. And moreover, that the opioid epidemic has just gotten worse over the pandemic in the last few years. So why is the brain a promising target or why might we think pain exists or lives in the brain? There is a wealth of literature, as I'm sure most of you are aware or many of you, from neuroimaging studies and humans from animal studies. Going back from at least the 1970s and more recently, FMRI and pet
studies trying to identify what's the locus or is there a locus for chronic pain in the brain. Multiple studies have demonstrated that there's no single region in the brain, there's no pain center. There's no single region that really harbors chronic pain as there may be for other senses. Chronic pain truly I think is one of the most fundamental experiences an organism can have. But also fundamentally one of the most complex in terms of its representation in the brain. So even though pain has been studied for many decades, most evidence in the literature in imaging studies comes from healthy folks who are exposed to acute or experimental pain. It's clear that there's unique signatures that you can
predict in an individual's pain report from the study from Tor Wager from Kathy Bushel's[ph] group, and, more notably that expectation and it's an influence on pain overlaps with opioids targets in the brain. And particularly in the first kind of part, I'm going to describe why we focused on the anterior cingulate cortex and the orbital frontal cortex. In general throughout the neuroaxis, from the brain to the spinal cord, to the peripheral nerves, in the last 70 years, neurosurgeons, neurologists, various clinicians have attempted to lesion or pass electrical current in an attempt to relieve patients suffering. Here's a great
review article showing in many areas that in red areas that have been commonly lesioned or in green areas that are commonly stimulated, there's a couple of errors but you could see them. Lesions is clear. When you lesion the target, it's not the same as stimulating the identical target. So we still, I think, don't understand fully why or how electrical stimulation might be able to provide a pain relief, but it's clear that it's not just inhibition or knocking out a particular brain region. Foltz and White were some of the first surgeons to actually identify the anterior cingulate cortex as a region that may be pain relieving. And they put relief in quotes because interestingly, they noted that patients after ablation of the anterior cingulate cortex reported perhaps feeling the same intensity of pain, but not being as bothered by it. So there's an interesting distinction or dissociation between the bothersomeness,
the unpleasantness of pain versus the intensity of pain. Brain stimulation, as I mentioned, has been studied for many decades. The first attempts were probably in the 1950s or '60s by Mazars in Germany. But contemporary approaches, I highlight here, started I think in the early seventies, Hosobuchi and Adams, actually UCSF, used thalamic stimulation for the treatment of anesthesia dolorosa. Since then, multiple other groups have attempted to find targets
as well as patient populations that might be amenable to brain stimulation, to relieve pain that's otherwise intractable. And to date, there's only one randomized control trial and that occurred in 2017 by Scott Lempa and [UNINTELLIGIBLE] group, which had a clinical negative outcome after stimulating the ventral striatum and the anterior limb of the internal capsule. So we understand that pain has multiple dimensions, and we make an attempt, often a reductionist attempt to assign these functions of somatosensory, affective, and cognitive to different circuits. But it's clear that the brain doesn't operate via a labeled line approach. It's clear that single brain regions don't perform a particular function when it comes to pain. People like to say the ACC supports the affective dimension of pain,
but we know that this is not true, strictly speaking, that truly that there's a network integrative mechanism that requires widespread circuits across the brain. So we still don't understand where in the brain to stimulate to release pain and the optimal targets knowing that would help us develop a therapy. Targets have worked well for some individuals actually lose efficacy over time and there are still pain syndromes that don't respond to any therapies that we have available. So the motivation for our study is essentially to figure out
one, can we identify biomarkers, can we understand where in the brain. Even though we understand that pain representations are widely distributed across the brain, can we understand or can we try to see if it's even feasible to track pain signals in the brain for the actual use case of real-world chronic pain as opposed to experimental pain? And then more ambitiously, can we use these signals to drive a closed-loop controller similar to a thermostat? The easiest or most simple version of a closed-loop controller. When the temperature goes up, the device turns on. In this case, we wanted to ask, "Can we have an on-demand controllable stimulation that might be pain relieving in response to real-time biomarkers?" So the study that we recently published, surprisingly, but after a lot of work, we were able to actually provide a proof of principle that yes, we can actually identify chronic pain biomarkers in the real world. And how did we do this? So in four subjects who enrolled in a deep brain stimulation trial using the Activa PC+S device, they had various pain syndromes. Three of them had
post-stroke pain. One of them had phantom limb pain. The subjects were implanted with special electrodes and a special device, the PC+S device, targeting the anterior cingulate cortex and the orbital frontal cortex. These devices allowed us not only to stimulate, which we didn't report in this paper, but most importantly for this paper, they allowed us to record neural activity at key points of the day. So patients, actually, over the course of many months, multiple times a day, ranging from three times a day to five times a day, would report their pain scores. They report a visual analog score, a numerical rating score, or McGill pain questionnaire, through an online survey. These black dots
here show an example patients of pain scores as they fluctuate over the course of 120 days. You could see that the pain score fluctuates above the minimal clinically important difference for VAS, and most uniquely, every black dot not only represents a pain score, but also represents a simultaneous brain recording that was captured when the patient pushed a button on the remote control to capture a 30-second snapshot of local field potential recordings from the anterior cingulate cortex and the orbitofrontal cortex obtained through implanted permanent electrodes. So here, we have accomplished this by using this research grade device. It's not commercially available, although there is are a couple commercially available devices that can accomplish something similar. But as you can see in red we show that the four contacts are in the orbitofrontal cortex, and there's four contacts in the anterior cingulate cortex. This is an x-ray showing the kind of construct of the electrodes connected to the recording and stimulating devices implanted in the chest. Across these four patients,
the electrodes were mostly distributed for the anterior cingulate cortex in the rostral ACC areas, I think popularized by TPO disease and other folks as a possible candidate for stimulation target. And here you can see the O F C, it's really the medial O F C. Also, in other studies, these areas has been referred to as the ventral medial prefrontal cortex in F M R I studies. So it's important to note that. So this paper, this report really focused on, all right, can we identify biomarkers by having patients report pain multiple times a day? And their stimulation was off, by the way. And then what we tried to do is continue the home recordings and optimize their stimulation, and those studies are ongoing. So, for the purposes of biomarker identification, what we did was we took each 32nd snapshot recording, here represented as a vertical. It's a vertical line across 250 recordings in the vertical line. You see the neural L F P power spectra, and it's Z scored. So high power in a particular
frequency from zero to 100 is represented as yellow, and low power is represented as blue. This particular graph is sorted such that the corresponding pain score that corresponds with each neural recording is shown in white circle here. So we sorted all of the neural recordings from lowest pain score reported, which is about a 45 or 50 out of a hundred to basically 80 out of a hundred. Patients here, we could either seek to predict the
exact pain score or we could try to predict a dichotomized pain score, for the purposes of closed loop, implementation, where we want to basically develop a thermostat. It's actually more useful to dichotomize the pain score because you can ask, when the pain biomarker passes a certain set point or threshold, you can have the device turn on. Again, the simplest implementation of an adaptive, brain stimulator. So if we dichotomize the pain scores based on their median pain score, and then if we extracted features that is the average power in various frequency bands, delta, theta, alpha, beta, gamma, et cetera, we asked two questions. We asked if we parcellate the data, we just sub-select the data from a certain brain region or a certain hemisphere. How informative is that neural data in predicting or classifying high pain versus low pain? And number two, we asked, can we use different methods, like linear discriminant analysis or state-based model, can we use different machine learning methods and how well do they perform compared to one another? So using, for our use case, as I mentioned, classification machine learning methods classifying high pain versus low pain in four subjects. And again, they're numbered CP one to four, all
those four different patients, believe it or not. We could actually classify using various brain regions using activity from only one hemisphere in the AC C or using activity from only one hemisphere in the O F C. In multiple patients, we could actually classify, we could accurately predict above chance whether they were going to be in a high pain state or a low pain state. And this is cross validated with leave one out. We did surrogate matching to obtain P values to make sure these are significant. But the most striking observation is that you could actually detect biomarkers in the wild, so to speak. When patients are
living their life, they're walking their dog, they're driving their car, we could actually accurately predict across all subjects using even the data from a single, brain region, whether they were going to be a high pain state or a low pain state. The most common area, actually the only area that seemed to generalize across all subjects, appeared to be the orbitofrontal cortex, but only when it was on the contralateral side of their usual pain. It's still an open question, whether pain is, laterality is, how to put it laterality is important in the same way it is for sensory systems, like touch or vibration or like it is for motor systems. But here it appears that the contralateral hemisphere, O F C was the common brain region that was successful in predicting chronic pain across patients.
We then wanted to compare it to what's mostly studied in the literature, acute pain state. So acute pain state was actually less reliable. We did a common task that's done quantitative sensory testing where we vary different temperatures on a thermo calibrated to each patient, when we use the same method of analysis. Interestingly, we could only successfully predict in two patients whether they were in a high pain state or low pain state. And again, this is not chronic pain, this is experimental pain. Interestingly, we could only predict the experimental
pain in those two patients when the stimulus was applied to the side of the body, that the usual chronic pain is also occurring in. What does this mean? To speculate a little bit, I think this might, in a way, I think of this as chronic pain may cause the brain to over represent the area of the body that's in pain. And this might be why, there may be a stronger signal or a higher signal to noise ratio for that body side, that body location, that body part, even when we're looking at experimental pain. So we actually looked in the models and actually tried to understand how do the different features vary. Again, we found that the common feature across all subjects for chronic pain appear to be delta frequency activity in the contralateral, cortex, that was the most discriminating feature of whether they were going to be in high and low pain. Really for acute pain, it looked
like the ACC features were actually more important. And, this graph basically just shows, whether or not feature weights for A C C or O F C were more important to try to see if there was a difference. And it seemed like there was a difference. Even the time course of the neural signals, was different. For high pain versus low pain groups within a patient, we looked at, across all the recordings, when the patient was in high pain, a high pain state, was that delta frequency or whatever other frequency, was that elevated for a long time? Did that come and go very rapidly? It appeared for chronic pain states. Whatever frequency discriminated high versus low pain, it actually, had a sustained change. It was
either increased for many seconds or decreased for many seconds. For acute pain, it actually seemed to fluctuate much faster on the order of hundreds of milliseconds. And again, this is only four patients. It's a big limitation. But the question now is can we use these insights of OK, we can actually, as a proof of principle, I think we're just scratching the surface of whether or not we can actually track, one we we're showing a proof of principle that, that we can track chronic pain in the real world. Now the next question is, can we actually use it to influence pain, to improve, people's lives and to produce pain relief? So in summary, spontaneous fluctuation of chronic pain can be tracked by converging metrics or direct cortical recordings can actually track clinical chronic pain state. Acute pain was harder
to detect. And last but not least, there may be overlapping biomarkers, but it's clear that our intuition, that chronic pain is not just a more enduring version of acute pain. It's not just a more enduring version of experimental pain. It's really, its own beast, so to speak. We provided a proof of principle in this study. And last but not least, I'm going to spend
about a minute or two just going over the current studies in progress. So I told you that the A C C and the O F C were good biomarkers or good locations for detecting biomarkers across subjects, particularly the O F C. We did find, and we're about to publish this, that stimulating those regions did not always result in pain relief. So we actually opted for a more exploratory trial where we used stereo electrodes probing multiple brain regions such as the insula, such as the somatosensory cortex, the periaqueductal gray, other regions, the dorsal lateral prefrontal cortex. We perform a systematic inpatient trial where we stimulate patients for 10 days in the hospital. And that's a picture of a brain here with all the electrodes in it. All these electrodes come out after 10 days. If the patient had
more than 50% relief, we implant them with a permanent device, targeting the best areas for stimulation based on the inpatient trial. And then we also implant the best areas for biomarkers based on the inpatient trial. And then we try to implement the biomarkers as well as the optimal locations into a closed loop paradigm. So we've recruited all of our subjects so far. Six subjects have undergone this invasive mapping trial. And here's the body pain maps that they've drawn. Here's an example, we're not only decoding classification,
we're not classifying pain state, we're decoding the actual pain state in this case. And I think the difference was you need many more brain regions to integrate signals across distributed networks. And you can actually see that the ground truth on the X axis, is very, quite well predicted by the predicted test points. Using a lasso regression model on the y axis mood was much easier to predict, believe it or not. So we take these features that were the most important for prediction, and we count them up and that's where we decide what our recording targets are going to be. And similarly, here's an example of a patient
and these multiple body map animations show over the course of 10 days, her horrible pain on one side of the body from post-stroke pain was actually almost completely resolved, and it was almost completely resolved through stimulation. And here we see, we stimulated over 30 different sites ranked by the amount of relief reported by the patient. Again, z scored worst relief on the left, best relief on the right. We identified a new brain region that we're about to publish. And again, the intensity is inversely related to the relief,
which is good or should be expected. So compared to Sham, we find the optimal stimulation targets during the trial period and implant them. Here's an example very briefly of what it looks like to implement biomarker driven feedback controlled or biomarker feedback controlled on demand brain stimulation at home. Here's one patient over one week, and this just ended
last week or two weeks ago, July 26th, and you can see that the stimulator is ramping up and we have a sleep aware stimulator that turns off at night based on a sleep biomarker. And basically, the stimulation's provided when the pain biomarker is actually elevated. And so the patient's receiving not stimulation on all the time, but honestly as needed throughout the day, if their pain is lower in the morning, stimulation will virtually be off in the morning. And the pain scores that they report here in orange are dramatically lower. So they're reporting pain scores on the order of two to 10, 20 to 100 in the VAS, in the McGill pain questionnaire is the last column you're seeing pain scores of 13 or nine or below. The baseline for this patient was six, seven and often had days of eight out of 10 pain.
And now they're reporting, on average, one to two out of 10 pain, which is really remarkable. And you can see the state switching, occurs on the order of many minutes or hours. So last but not least, when these patients draw their pain body diagrams, you can see that at baseline where they had horrible pain represented in red, blue representing mild to moderate pain with the trial period, we are able to dramatically reduce their pain by finding optimal sites. And we could replicate this using both open loop stimulation, but even
more dramatically with closed loop stimulation that uses much less current and provides on demand stimulation in real time. Thanks so much again to everybody and I apologize for going over time, but I'm happy to take any questions. LANGHALS: Cool. Thanks Prasad. And thanks to Dr. Wagner as well. At this point we have about 15 minutes or so available still for questions. So for those that have questions,
as a reminder, place them in the Q and A and we'll try and get through as many of them as we can. So we already have a few in there already, so we'll start with some of those. So, Dr. Wagner, how do you account for the significant placebo effect in both your studies? WAGNER: Well, I think the key thing is that we're separating from the placebo effect, and I would actually be unhappy if we didn't see a placebo effect in these patients, especially in the pain patients. It's quite common across the non-invasive brain stimulation studies that you will see a placebo effect in the sham conditions if you blind the patients appropriately. And I like to say pain is in the mind, so seeing the impact of a placebo to me is OK, as long as we are separating from it and showing a significant separation from the placebo effect. LANGHALS: Thank you. Dr Shirvalkar, great presentation. Do you believe that modulating
the activity of the OFC could also be a biomarker for therapeutic efficacy? SHIRVALKAR: It's a great question. Yes I do, simple answer. I didn't show this, but when we find or when we actually are able to find targets that work for patients, we actually - we've looked in the OFC, the ventromedial prefrontal cortex. And the good news is that the biomarkers that we identified in the Nature neuroscience paper, as far as we've shown, there are only correlations. But the good news is they seem to be causal as well in the sense that if you move them in the correct direction, it does seem to actually result in pain relief. So I think, one, it could be a biomarker factual pain treatment. But there's another related point, and I think it's really important. Samir Sheth's group
and other folks are working on brain stimulation biomarkers for prognosis. Can you kind of understand when you stimulate, there may be other epiphenomenon that happen? Signals that change in other regions that tell you whether or not that's going to be a good target. And that's kind of a separate question. But at the end of the day, I think OFC ventromedial prefrontal cortex actually is a very promising area for biomarkers to modulate those signals as a predictive feature for brain stimulation. LANGHALS: Thanks. Back to Dr. Wagner. In your phase two clinical trial, are you using the opioid craving scale? WAGNER: We are using, we're going to use VAS craving. We're going to use the three item
craving scale, and the OCDUS, the obsessive compulsive drug use scale for our craving. LANGHALS: Dr. Shirvalkar, did you identify handedness in your pain subject? Left versus right. And I'll just add a follow-up, and was there any sort of effect that you've noticed so far in the studies? SHIRVALKAR: That's a good question. We did identify handedness. I don't know if you're
a neurologist, but spoken like a true neurologist. It's the first line in our assessment. They were all right handed by the way. In our second study, our HEAL funded study, there's one left handed patient. And I'll say we've not analyzed that data yet, so I'll let you know,
Nick and everyone else. LANGHALS: Back to Dr. Wagner. For the yes stim, what is the process of adjusting stimulation parameters to a participant? Are there any long term risks for the yes stim therapy? WAGNER: For the trials that I've presented on and the trials that we're conducting, we're providing a fixed dose of stimulation. It's defined in advance. We did recently publish
the journal of big data though that a method for optimizing, or a method that we have under production for optimizing and adjusting the parameters for the participant where we would potentially modulate the parameters based on biophysics models that would be MRI derived field models of the dose of stimulation at the target site correlated with baseline parameters from the patient with essentially statistics and predictive models. Now for long term risks, we have not identified any long term risks. The current safety profile is fairly equivalent to TBCS in what we have seen. LANGHALS: Thank you. Back to Prasad. Provided your current studies go as planned, when would you hope your treatment approach could be available to patients? And who do you think would be the patients best suited for it? SHIRVALKAR: That's a great question. I get that a lot. And so you become very realistic and very grounded. Reality slaps you in the face as you try to do clinical trials. If
we can move our phase zero, phase one trials in the next five years. And then if you could partner with the NIH or have a company to run phase three trial five years after that, I am hoping that by 2032, 2033, this could be FDA approved. One of my key gals in my lifetime is to try to figure out how to make PBS for pain good enough to get it FDA approved. 10 years is realistic, but of course timelines change. I guess the - sorry, what was the
second part of that question? LANGHALS: And which patients could be best suited for this? Kind of where might this fit in to the availability of other treatments that are in development or currently available? SHIRVALKAR: I think of brain surgery or anything involving putting things in your brain is an option of last resort. Our trial is truly a therapy of last resort. Right now we're recruiting folks who have chronic neuropathic pain. We define neuropathic pain nociceptive, visceral, neural, nociplastic. That being said, many of our patients with neuropathic pain, they have overlapping nociplastic pain, they have degenerative spinal disease, they have facet arthritis. They have knee replacements and they still have knee pain that's inflammatory. And they get benefit for the DBS. It's clear it doesn't just work for neuropathic pain.
I think multiple pain types are going to be amenable to DBS in the future. That being said, again brain stimulation is very invasive. If we could do this non-invasively, that would be very awesome. So far to my knowledge, and believe me, we're trying. All non-invasive therapies - and Dr Wagner, thanks to you. He said it really well. I think you called
them online effects and offline effects. We call them effects while stim is on, and then wash out effects when stim is off. There is a wash out effect as far as the non-invasive brain stimulation. If non-invasive brain stimulation, the big obstacle is you can have an enduring effect on a reasonable time scale. We have patients come back to the clinic to repeat injections every three months. If you could have non-invasive stim last three months,
that would be amazing because that would be better than putting something in your brain. But right now there isn't, and so we're still trying. LANGHALS: Thanks. Dr Wagner, can you elaborate on how the patients in the placebo group were also adapted with a device during stimulation or lack of stimulation? WAGNER: If I understand the question correctly, again, seeing a placebo response in chronic pain patients is not unreasonable and something that is anticipated. I'll tell you, though, what we generally see across our pain studies is the placebo effect when we have longer follow-up period goes away rather quickly. You'll see a maximum placebo effect generally
on the last day of the placebo stimulation, and it generally goes away. While you see the more sustained effect of the active stimulation that has that offline effect, or a longer much longer washout period than you would see in the placebo group. We're seeing in the impact of patients six and eight weeks post stimulation in that, while the sham patients will really attenuate rather quickly in most trials.
LANGHALS: And Dr. Shirvalkar, this is probably a follow-up related question, is do you envision a future way to translate some of these neuro biomarkers that you're finding into a non-invasive treatment? SHIRVALKAR: That's a really good question, and I've thought about this a lot. And for me, I may be - and please correct me or educate me if I'm missing something. The logical step seems to be if we can find an invasive biomarker - we're doing EEG studies as well. You might think of F in years, or something like that for the frontal cortex or cortex. The idea
is validate, can we non-invasively detect the same biomarkers that we detect invasively? If we can do that, then we have to show or test actually, can we non-invasively modulate those biomarkers that we can modulate invasively? Because we're doing most of our work invasively, it's really hard to shock them to non-invasive scenario. But if they existing basically, the hope is the same way that people were skeptical of FMRI until it was shown that FMRI, bold signal actually does reflect actual population neurons spiking. People did electric recordings with FMRI. If we could demonstrate something with a similar study, there will
be a lot more confidence from me. There's a lot of technical hurdles that we have to overcome. LANGHALS: No problem. And I guess back to Tim, have you looked at user satisfaction
with your device so far? WAGNER: We've started to add user satisfaction components into some of our ongoing studies. We didn't have that in some of our early studies, and I wish we did. We do have testimonials and such, but not a validated user satisfaction metric that we'd use.
LANGHALS: And back to Prasad, very interesting presentation. With the biomarker closed loop feedback stimulation, have you thought about potential unintended changes in the neural circuit? Changes could be either negative or positive in response to the stimulation. SHIRVALKAR: Yes, absolutely. One of the biggest fear, unintended consequences is habituation or tolerance. It's so sad or scary. But even a spinal cord stimulation or other modalities of nervous system stimulation. It seems like the nervous system often gets used to, or
habituates, or develops tolerance to electrical stimulation. And it's not only due to the formation of scar tissue or some kind of mechanical barrier. It's some kind of rewiring or plasticity. One thing that we're trying to understand is if you can have a stimulation protocol that improves pain, that's great. What are the plastic changes that are happening to that over time, and how can you stay ahead of them? That's a big one. Number two, what's
interesting in the biomarker sense. If patients get sick, if they're ill, if they get COVID, if they change medications, if they take a different blood pressure medications, its biomarkers are affected. And so right now we require them to be on a stable dose of medications. But there's extreme sensitivities to even things like time of day. Finding biomarkers
that are robust to confounding factors is going to be an important consideration. LANGHALS: And back to Tim, this was a follow-up for one of the earlier questions. What made you choose the OCDU scale over the OCS? WAGNER: The three item craving scale, we are using UCDUS, we're using n of that craving. That is the current plan, and had to with conversations with various people. Our goal
is ultimately approval of the device, and looking at what has been used previously. And I'm sure the questionnaire has is there's not a validated craving scale. And we felt this was the most comprehensive paradigm for our current trial. LANGHALS: And so that's the last question from the audience. I'll as moderator, take liberty and ask one more to both of you. Given kind of the vast array of kind of dosing strategies for these sorts of stimulation, whether invasive or non-invasive. How do you see that being
better optimized over time to determine how often they're needing to come in to get the therapy? And what might be that optimal target for each of the strategies? WAGNER: Please go ahead. I'll chime in after. I think it's a great question. SHIRVALKAR: Yes, me too. It's funny, the ideal situation would be if we could figure out what is the plasticity? The maladaptive plasticity that causes chronic pain in the first place. If you can figure out if we put electrodes in the brain or maybe not in the brain, can we reverse this plasticity? Can we temporarily treat for a period of a month or two months? Is there a time limited treatment by which we can deliver electrical stimulation and then take the device out all together? That would be the ideal. Can we reverse the plasticity?
As we know, nature is a strong force. And so even a few seconds of trauma or a moment of trauma in someone's life can last decades or a last time. It can take a lot of effort, a lot of time to undo. It's a really challenging question. Right now the state of the art of brain stimulation, I'll say we've had patients which you could stimulate using adaptive stimulation. They may receive two to three minutes of stimulation. And there's some patients who can actually go 24 hours, and have so called washout period or offline period where they're better. They
may only need a few minutes of stimulation a day. Can we actually get it to the point where it would cure them? I think that would be the ideal. But so far, I think we need more mechanism studies to characterize what is that plasticity that goes on? And start even asking the question, how can we undo it? WAGNER: And to a great answer, and I agree completely. And one thing we've contemplated is, is there a way to block the transition from an acute pain to a chronic state? And can you block chronicity? Can you identify those patients who are more prone to flipping from acute to chronic? And so we have a few things underway working on that. But as Prasad said, it's a very difficult problem. It requires quite a bit more exploration. But that's one
of the key things that could be done. And that ultimately comes to optimizing the therapy for each individual patient because pain is subjective. And every patient doesn't have a unique zero and one output in pain. We're doing our best to model the pain response based on baseline characteristics of the patient, whether it be imaging based, whether it be quantitative sensory testing based, whether it be subjective questionnaire instruments.
We're trying to use everything that's in our kind of wheelhouse to identify those and best optimize the therapy. LANGHALS: Thanks again to both of our presenters today. And I'll turn it back to Diana to wrap us up.
MORALES: Thank you everyone for attending this session. It was fascinating and exciting. And we look forward to hearing about progress in the future. I hope everyone will be able to join us for our next webinar, which is on Friday, September 8 at 2pm Eastern Time, and it will focus on data driven solutions for pain and addiction. Again, thank you so much. Happy Friday.
2023-08-10 07:10


